zwnews.com Reporter- Lovemore Lubinda
Campaigns against HIV and TB in children in Zimbabwe may yield less unless drugs friendly to children are provided.
People with children living with HIV or affected by TB have expressed concern that it is often difficult to administer a set of medicines to children who suffer from the diseases.
“The treatment itself is so difficult to give to my children because I don’t know if I am giving the right dosages to them or not,” says Sithembile Makheleni a resident of Hopley settlement in Harare, who has two children 6 and 9 years on TB treatment, “The medicines taste so bad that my children often refuse to take them.”
Makheleni says she always has to be around fearing that her children may be given wrong dosages.
Currently, children from ages 0-5 have to visit the health centers where they are weighed and given their medicines, while those older have to rely on the parents and caregivers. In many areas of Zimbabwe, it has placed a burden to parents who often have to walk long distances to receive their medicines and improvise when giving the dosages.
Advocacy group Zimbabwe National Network of People Living with HIV (ZNNP+), submits that there have been some challenges in giving the medicines to children.
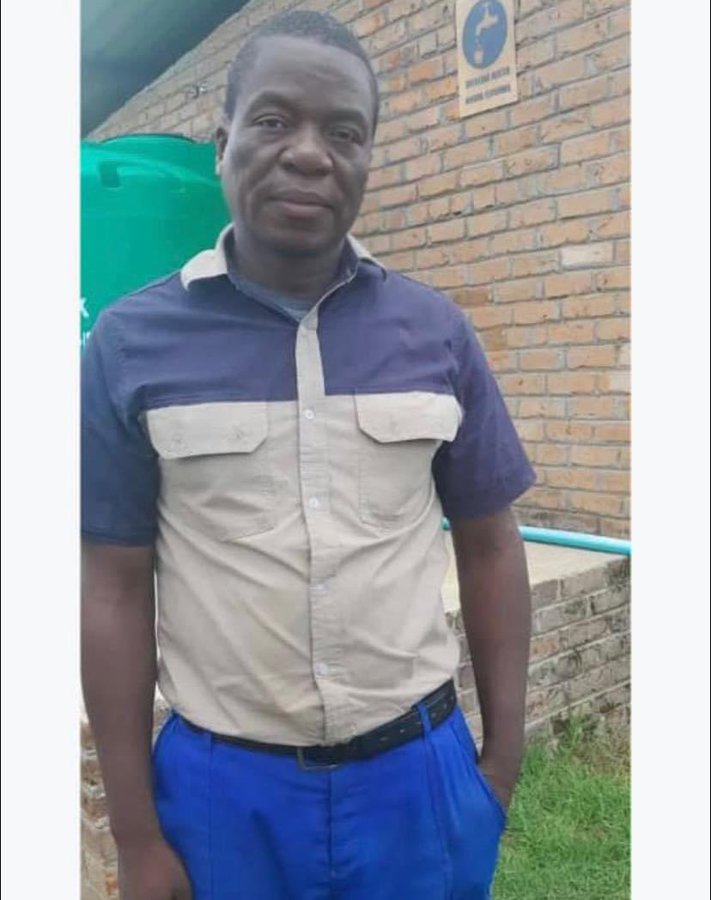
Dagobert Mureriwa director of ZNNP+ says many members of his organization are insisting on drugs that are tailor-made to suit children, clear and understandable to parents and other caregiver and peers.
“Parents and care providers have to approximate the correct dose for a child. They have to crush or chop available drugs, and piece together the treatment regimen. Splitting TB pills, usually results in imprecise dosing. Coupled with the bitterness of the pills, makes the treatment journey even more difficult for children and their families. Such challenges can also make treatment less effective, leading to poor health outcomes and the development of more difficult to treat drug-resistant TB in children,
“Tied up with the uptake of a combination of at least three antiretroviral drugs by children with HIV-TB can prove too difficult resulting in children abandoning treatment,” says Mureriwa.
HIV-infected children with TB require antiretroviral therapy (ART) and co-trimoxazole preventive therapy in addition to TB treatment.
Charles Sandy, deputy director of HIV and TB unit in the ministry Health and Child Care, acknowledges that the ministry of health recognises some of the challenges inherent with use of some of the medicines used on the managed of TB and HIV in children.
“In the management of TB the fixed dose combinations that we currently use are not appropriately calibrated and as such may result in under dosing in children in some weight bands,” says Sandy.
“The Ministry recognizing this development, is phasing out the old formulations that are currently in use in favour of better calibrated ones which will reduce the likelihood of under dosing,” he says,” We expect to have the new formulations in the country by the end of the year and all pediatric patients diagnosed from January 2017 will treated using the new formulations.”
He revealed that the World Health Organisation (WHO) and TB Alliance have announced the development of better formulated childhood TB Medicines in 2015 at the Lung Conference in Cape Town. These new formulations are now available for procurement by countries.
Sandy says in HIV treatment the challenge is mainly with the storage of Lopinavir/Ritonavir syrup which requires refrigeration. The other formulation currently available for Lopinavir/Ritonavir is tablets which are difficult swallow for small children. There are pellets of the Lopinavir/Ritonavir that have been developed and the ministry would to introduce these in order to mitigate against the challenges associated with use of the tablets and syrup. The Ministry is currently conducting feasibility studies on the use of the pellets to appropriately inform recommendations on administration and to assess their acceptability among children and care givers.
Both the MoHCC and health partners believe that the right medicines and doses and will increase adherence and save more lives.
In 2010 WHO guidelines recommend fixed-dose combinations (FDCs) for the treatment of TB. FDCs simplify the treatment regimen for patients, causing fewer side effects and reducing the pill burden.
According to the international health NGO TB Alliance, Child-friendly medicines improve the daily lives of children and their families struggling with TB-Six month is a long time to take medicine. But the availability of treatment that tastes good and is simple to provide will ease the daily struggles of children and care givers.
TB Alliance and its partners announced today the availability of child-friendly tuberculosis (TB) medicines in the correct doses. The improved treatments are the first to meet the dosage guidelines set by the World Health Organization (WHO) in 2010. They are dispersible and palatable, simple to administer and affordable. The availability of these products is a result of a project largely funded by UNITAID.
The WHO says at least 1 million children become ill with TB each year and 140,000 children die of this curable disease. In 2014, 81 000 children died of TB, and there were an additional 55 000 TB deaths among children who were HIV.
TB now ranks as the world’s leading infectious disease killer along with HIV. The disease is curable with treatment, which consists of multiple drugs and must be taken for a minimum of six months. Children need different doses of TB medicines than adults.
The new TB medicines are fixed dose combinations (FDCs) of the three most commonly used drugs to treat drug-sensitive TB (rifampicin, isoniazid, and pyrazinamide). These are not new drugs, but rather improved formulations that are dissolvable and flavored so that they are simple for providers and parents to administer and easy for children to take. The FDCs are rifampicin + isoniazid + pyrazinamide, which are used for the initial two months of treatment, followed by four months of rifampicin + isoniazid. The formulations are in the process of being prequalified by WHO but are now available under the WHO’s Expert Review Panel mechanism.